World-Class Technology That Saves You Money
World-Class Technology That Saves You Money
you money while providing uncompromising safety.



Eight of the Top 10 U.S. Hospitals* Use VanishPoint Syringes
Savings, you say?
Medication Savings
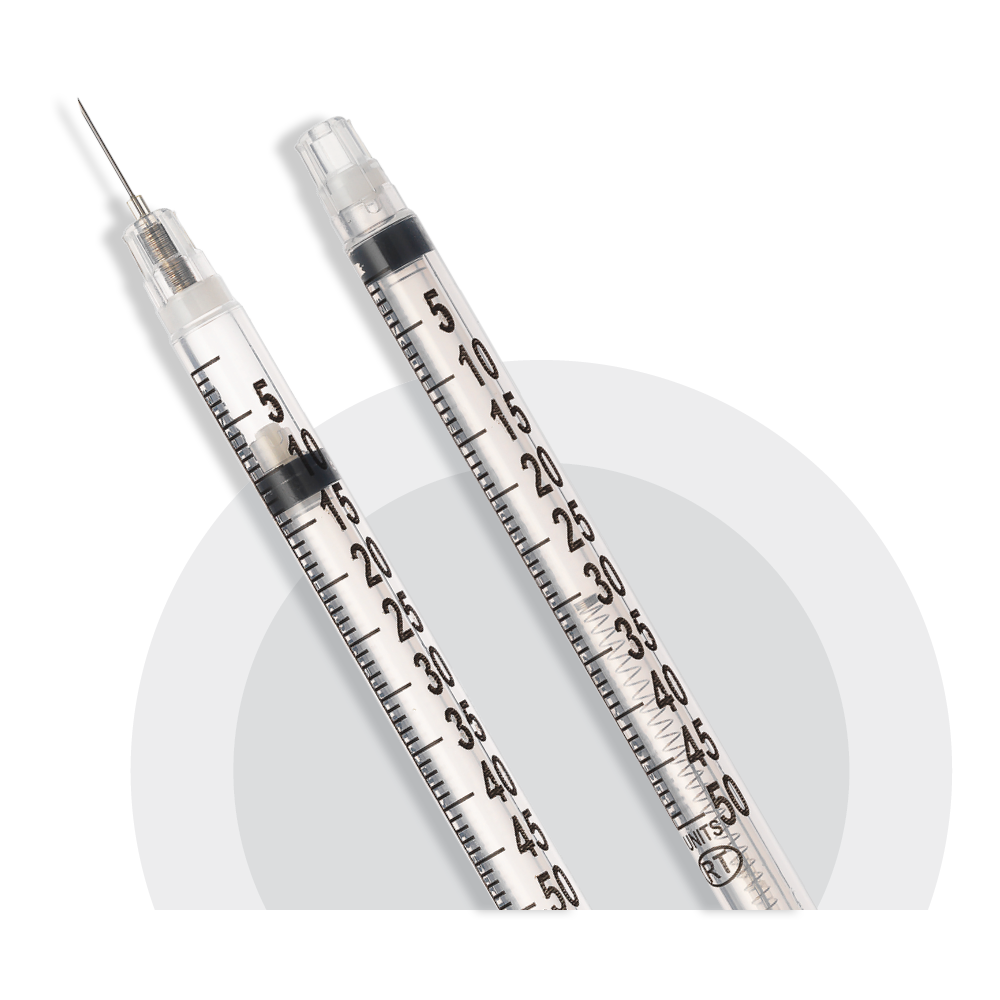
Standard syringes contain residual medication after use, and that medication is wasted. VanishPoint Low Dead Space (LDS) syringes give you the ability to obtain an extra dose from a multi-dose vial of medication while providing precise and accurate dose delivery to patients.
Time is Money
We all know that time is money. We kept that in mind when engineering our products. Automated retraction devices save time by streamlining the injection process. And the VanishPoint Syringe’s superior needlestick injury protection saves money for healthcare facilities.
Disposal Savings
The VanishPoint Syringe has an attached needle that prevents unnecessary (and expensive) needle changes. After activation, the syringe occupies significantly less space in a sharps safety disposal box. As a result, healthcare facilities can reduce their waste management costs, including the number of boxes needed, and the transportation and disposal costs for the full boxes.
Needlestick Prevention
Needlestick injuries to staff members can result in significant costs, including those for post-exposure prophylaxis, testing, treatment, follow-up care, workers comp claims, staffing shortages, and potential legal expenses. By using RTI safety products, healthcare facilities can substantially reduce the risk of injuries to employees, along with reducing costs.
